- Visibility 158 Views
- Downloads 23 Downloads
- Permissions
- DOI 10.18231/j.ijced.2022.025
-
CrossMark
- Citation
Study of clinicohistopathological correlation of skin adnexal tumours
Abstract
Background: Appendageal tumours (Appendageal tumours) are neoplasms which differentiate towards or arise from pilosebaceous apparatus, apocrine gland or eccrine sweat glands. Overall incidence of Appendageal tumours is low, yet they can be challenging to diagnose.
Aim: The study aims at determining the frequency, profile, and distribution of skin adnexal tumours and association of their distribution with patient’s age and sex.
Materials and Methods: Cross-sectional descriptive study, conducted over 1-year period. All clinically suspected cases of Appendageal tumours were evaluated and subjected to histopathological examination. Confirmed cases of Appendageal tumours were finally analyzed.
Results: Out of 43586 new patients attending OPD, 64(0.14%) cases of Appendageal tumours were suspected. And 60 underwent histopathological examination. Histopathology was confirmatory in only 42 (70%) cases. Out of 42, the hair follicle tumors comprised of trichoepithelioma 18/42(42.85%), trichofolliculoma 1/42 (2.38%), pilomatricoma 4/42 (9.52%), and trichilemmal cyst 4/42 (9.52%). The sweat gland tumors are comprised of chondroid syringoma 12/42(28.57%), hidrocystoma 2/42(4.76%) and syringocystadenoma papilliferum 1/42(2.38%). Females (61.90%) outnumbered males (38.09%) in our study population.
Conclusion: The incidence of benign skin Appendageal tumours is more as compared to the malignant ones as found in our study. Histopathology remains the gold standard for diagnosis of these tumours.
Introduction
Appendageal tumours (Appendageal tumours) are neoplasms which differentiate towards or arise from pilosebaceous apparatus, apocrine gland or eccrine sweat gland.[1] These tumors basically originate from undifferentiated pluripotent stem cells and finally differentiate to specific tumors influenced by genetics, local vascularity, and the microenvironment of the epidermis and dermis. Head and neck region is unique because of its rich distribution of pilosebaceous apparatus, apocrine as well eccrine sweat glands. It has also been previously documented that Appendageal tumours predominate over head and neck area.[1] Clinical diagnosis of different entity is often difficult, as most of the Appendageal tumours present as asymptomatic papules or nodules. Anatomic location, number and distribution of these lesions provide important clue to clinical diagnosis but histopathology is invaluable in conformation of the diagnosis.[2]
Majority of these tumours are benign[3], [4] and the malignant ones are usually irregularly shaped, solitary, rapidly growing plaques or nodules that have a tendency to ulcerate. Risk of malignant degeneration varies with individual lesions.[2] Local recurrence is well recorded but metastases is rare with the exception of the malignant eccrine and apocrine gland derived tumors and sebaceous carcinoma.[3] However, diagnosing some of these tumors has important implications, as they might be markers for syndromes associated with internal malignancies, such as trichelemmomas in Cowden disease and sebaceous tumors in Muir-Torre syndrome.[5]
The study aims at determining the frequency profile, and distribution of skin adnexal tumours and association of their distribution with patient’s age and sex.
Materials and Methods
It was a cross-sectional, descriptive study, conducted over a period of 1 year from November 2018 to November 2019. Total numbers of patients attending dermatology OPD were recorded and clinically suspicious cases of Appendageal tumours were evaluated. Histopathological examination was advised in all suspected cases and only those subjects consenting for histopathology were included for the study. Confirmed cases of Appendageal tumours were considered as the finally analyzable subjects.
Inclusion criteria
Patients irrespective of age and sex presenting with skin adnexal tumours willing to give consent for enrollment into the study, and In case of paediatric age group, those patients whose parents willing to sign the consent form.
Exclusion criteria being
Patients clinically diagnosed as having appendageal tumours but not proven histologically as having adnexal tumour. And Patients not willing to participate in the study.
Results
Among 43586 new patients attending OPD, 64(0.14%) cases of Appendageal tumours were suspected. And 60 underwent histopathological examination. Histopathology was confirmatory in only 42 (70%) cases, with an incidence of 0.096%. In the remaining eighteen patients, histopathology revealed either milia or epidermal cyst or basal cell carcinoma. In our study, 70% of clinically suspicious cases were proved to be of appendageal in origin. The hair follicle tumors constituted the largest group involving 26/42(61.90%), followed by the sweat gland tumors 16/42 (38.09%). The hair follicle tumors are comprised of trichoepithelioma 18/42(42.85%), trichofolliculoma 1/42 (2.38%), pilomatricoma 4/42 (9.52%), and trichilemmal cyst 4/42 (9.52%). The sweat glands tumors are comprised of chondroid syringoma 12/42(28.57%), hidrocystoma 2/42(4.76%) and syringocystadenoma papilliferum 1/42(2.38%) [[Table 1]].
|
Tumours |
Number (n=42) |
Percentage |
|
Trichoepithelioma |
18 |
42.85% |
|
Syringoma |
12 |
28.57% |
|
Pilomatricoma |
4 |
9.52% |
|
Trichilemmal cyst |
4 |
9.52% |
|
Hidrocystoma |
2 |
4.76% |
|
Syringocystadenoma papilliferum |
1 |
2.38% |
|
Trichofolliculoma |
1 |
2.38% |
|
Total |
42 |
100% |
Mean presenting age of our study population was 32.64 years (ranging from 11 to 55 years). Most common site affected was head and neck 31/42(73.80%) followed by trunk 9/42(21%), and upper limb 2/42 (5.20%)[[Table 2]].
|
Site of the tumour |
Number |
Percentage |
|
Head and neck |
31 |
73.80% |
|
Trunk |
9 |
21% |
|
Upper limb |
2 |
5.20% |
Female’s outnumbered (65.21%) males (34.78%) in our study population with the male to female ratio being 1:1.62[[Table 3]].
|
Tumours |
Number of tumours |
Male |
Female |
Male: Female |
|
Trichoepithelioma |
18 |
10 |
8 |
5:4 |
|
Syringoma |
12 |
2 |
10 |
1:5 |
|
Pilomatricoma |
4 |
1 |
3 |
1:3 |
|
Trichilemmal cyst |
4 |
3 |
1 |
1:3 |
|
Hidrocystoma |
2 |
0 |
2 |
0:2 |
|
Syringocystadenoma papilliferum |
1 |
0 |
1 |
0:1 |
|
Trichofolliculoma |
1 |
0 |
1 |
0:1 |
|
Total |
42 |
16 |
26 |
1:1.62 |
Discussion
The incidence of Appendageal tumours is very low and only 0.096 % of patients attending the OPD were found to be suffering from Appendageal tumours our study. Skin appendageal tumors differentiate along one or more adnexal line and their overall incidence is low in our Indian population.
Appendageal tumours are classified into 4 types according to their differentiation toward apocrine gland, eccrine gland, sebaceous gland and hair follicle. [6]
Importance of diagnosing Appendageal tumours lies in the fact that the presence of Appendageal tumours in some instances may lead to the recognition of a genetic syndrome, like Muir-Torre syndrome associated with sebaceous tumors, Cowden's syndrome with trichilemmomas, etc.[3] It is currently believed that Appendageal tumours are derived from cells that have the ability to differentiate toward any of the appendages. In many lesions, the differentiation is uniform and the tumor can be recognized and categorized based on its resemblance to a normal appendage or part of it. In other cases, the pluripotent cell may differentiate toward more than one type of appendage giving rise to a tumor that contains element of two or more appendage in varying degrees of maturation.[3] In our study, though such combined nature was not detected. The clinical appearance of appendageal tumor is mostly non-specific [1] and their diagnosis lie firmly in the realm of histopathologists. In the present study, 30% (18 /60) of clinically suspected cases were proved to be non-AT after histopathological examination. Milia were mistaken as syringoma, basal cell carcinoma as desmoplastic trichoepithelioma. Hence, these entities should be kept in mind before making a diagnosis of Appendageal tumours.
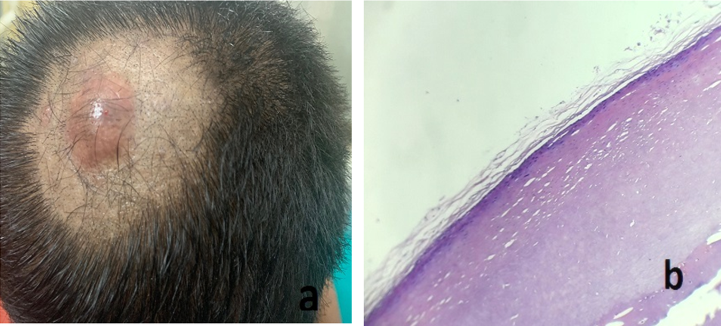
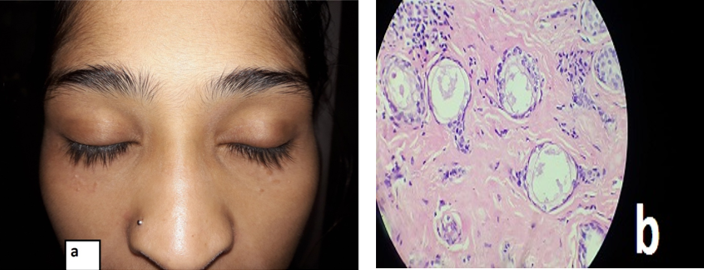
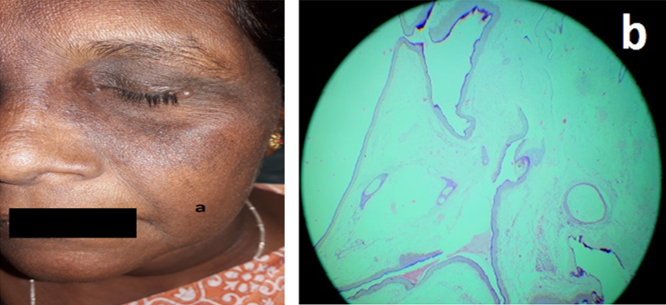
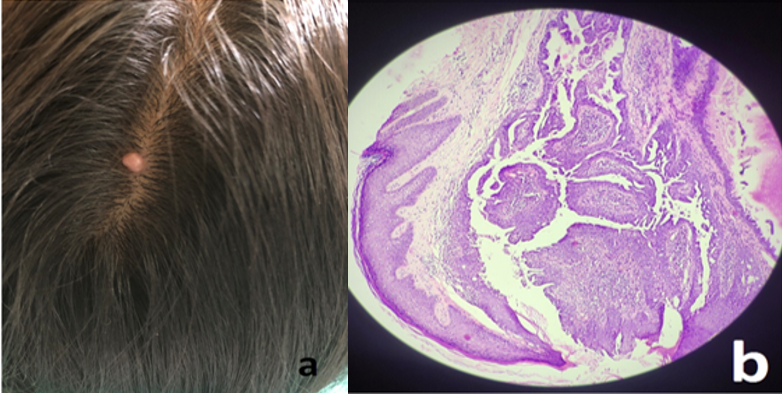
In our study, trichoepithelioma [[Figure 1]a,b ] was the most common hair follicle Appendageal tumours constituting 18/42(42.85%) and were distributed around nose suggesting that trichoepithelioma remains the primary differential diagnosis of Appendageal tumours centered around nose. Trichoepithelioma was found to be multiple and familial only in four cases, while solitary variety was found to be more common than multiple. Other hair follicle Appendageal tumours in our study were trichofolliculoma [[Figure 2]a,b] constituting 1/42 (2.38%), pilomatricoma [[Figure 3]a,b] constituting 4/42 (9.52%), and trichilemmal cyst [[Figure 4]a,b] constituting 4/42 (9.52%).



Among sweat gland tumours chondroid syringoma [[Figure 5]a,b] was the most common Appendageal tumours constituting 12/42(28.57%), hidrocystoma[[Figure 6]a,b] constituting 2/42(4.76%), followed by syringocystadenoma papilliferum [[Figure 7]a,b] constituting 1/42(2.38%).
No sebaceous gland Appendageal tumours were identified in our study. Incidence of benign tumours is more as compared to malignant cases. In our study histopathological features of malignancy was absent in all cases and supports the usual benign course of the Appendageal tumours. In present study, most common tumours were Trichoepithelioma and Syringoma followed by Pilomatricoma and Trichilemmal cyst.[7], [8], [9], [10], [11], [12]
To summarize the incidence of benign skin AT’s is more as compared to the malignant ones. Skin adnexal tumours can occur anywhere in the body; however head and neck region constitutes the most common site. Histopathology remains the gold standard for diagnosis of these tumours. The higher incidence among females of any age group than males.
Conflict of Interest
None.
Source of Funding
None.
References
- Mackie R, Calonje E, TB, SB, NC, CG. Tumors of the skin appendages. Rooks Textbook of dermatology. 7th Edn.. 2004. [Google Scholar]
- Stantaylor R, Prone JB, Kaddu S, Kerl H, KW, LG, et al. Appendage Tumors and Hamartomas of the skin. Fitzpatrick’s Dermatology in general medicine. 2008. [Google Scholar]
- Khandpur S, Ramam M, RV, AV. Skin Tumors. IADVL Textbook of Dermatology. 3rd Edn.. 2008. [Google Scholar]
- Samaila MO. Adnexal skin tumors in Zaria, Nigeria. Ann Afr Med. 2008;7(1):6-10. [Google Scholar] [Crossref]
- Tumoursuda KM, Doi T, Kosaka H, Tasaki N, Yoshioka H, Kakibuchi M. Sebaceous carcinoma arising in nevus sebaceus. J Dermatol. 2005;32(8):641-4. [Google Scholar] [Crossref]
- Klein W, Chan E, Seykora JT, DE, RE, Jr BJ, et al. Tumors of the Epidermal Appendages. Lever's Histopathology of the Skin. 9th Edn.. 2005. [Google Scholar]
- Bhat S, Prasad K, Bhat V, Shetty J. Clinicopthological study of cutaneous adnexal tumors in a tertiary hospital of South Iindia. Indian J Patho. 2016;3(4):649-52. [Google Scholar]
- Sharma A, Paricharak D, Nigam J, Rewri S, Soni P, Omhare A. Histopathological study of skin adnexal tumours-Institutional study in South India. J Skin Cancer. 2014. [Google Scholar] [Crossref]
- Saha A, Das N, Gharami R, Chowdhury S, Datta P. A clinic-histological study of appendageal skin tumors, affecting head and neck region in patients attending the dermatology opd of a tertiary care centre in eastern India. Indian J Dermatol. 2011;56(1):33-6. [Google Scholar]
- Suri J, Mahajan D, Koul KK, Kumari R. A clinicopathological Analysis of Skin Adnexal Tumours: Four Year Retrospective study. JK Sci. 2016;18(4):248-51. [Google Scholar]
- Nair L. A clinic- histopathological study of skin appendageal tumours. Indian J Dermatol. 2008;74. [Google Scholar] [Crossref]
- Jindal U. Study of Adnexal Tumours of The skin: A Three Year Study of 25 cases. Internet J Pathol. 2012;13(3):1-7. [Google Scholar]
How to Cite This Article
Vancouver
Budamakuntla L, Ansari MS. Study of clinicohistopathological correlation of skin adnexal tumours [Internet]. IP Indian J Clin Exp Dermatol. 2022 [cited 2025 Sep 14];8(2):114-117. Available from: https://doi.org/10.18231/j.ijced.2022.025
APA
Budamakuntla, L., Ansari, M. S. (2022). Study of clinicohistopathological correlation of skin adnexal tumours. IP Indian J Clin Exp Dermatol, 8(2), 114-117. https://doi.org/10.18231/j.ijced.2022.025
MLA
Budamakuntla, Leelavathy, Ansari, Mohammed Shahid. "Study of clinicohistopathological correlation of skin adnexal tumours." IP Indian J Clin Exp Dermatol, vol. 8, no. 2, 2022, pp. 114-117. https://doi.org/10.18231/j.ijced.2022.025
Chicago
Budamakuntla, L., Ansari, M. S.. "Study of clinicohistopathological correlation of skin adnexal tumours." IP Indian J Clin Exp Dermatol 8, no. 2 (2022): 114-117. https://doi.org/10.18231/j.ijced.2022.025
