- Visibility 315 Views
- Downloads 60 Downloads
- Permissions
- DOI 10.18231/j.ijced.2025.005
-
CrossMark
- Citation
Depression and quality of life among patients with dermatophyte infections at a rural tertiary care hospital-A cross sectional study
Abstract
Background: The relation between psychiatry and skin diseases is bidirectional. Despite proper drug compliance and adequate treatment, there are still recurrences. This has significant impact on mental health, which may cause psychiatric comorbidity, typically anxiety and depression. We have screened for the prevalence and severity of the same, to further understand this equation.
Aims and Objectives: To evaluate depression and assess its severity and association with dermatophyte infections in patients at a tertiary care hospital.
Materials and Methods: This cross-sectional observational study included patients with fungal infections from dermatology consultations. Basic demographics were collected, and the severity of depression and anxiety was evaluated using the Hospital Anxiety and Depression Scale (HADS) and Beck’s Depression Inventory (BDI). The Dermatological Quality of Life Index (DLQI) was used to assess quality of life.
Results: A survey of 183 dermatophytosis patients (88 male, 95 female) found the highest incidence in the third to sixth decades of life. Most had comorbid conditions, substance use history, and experienced one to six months of illness. Patients with itchy lesions had poor hygiene, contact with domestic animals, and irregular bathing. The Hospital Anxiety and Depression Scale indicated borderline anxiety and depression, with minimal to moderate depression. The Dermatological Quality of Life Index showed minimal to moderate effects, significantly impacting quality of life.
Conclusion: This study explores the mental health impact of dermatophytosis in India, highlighting its multidimensional nature and the need for a comprehensive understanding of its psychological toll.
Background
The field of Indian dermatology is grappling with a notable surge in dermatophytosis, a condition historically common in the country. Dermatologists report a significant shift in the clinical profile of patients with dermatophytosis, both in terms of quantity and quality. Determining the causes of this change is challenging, with uncertainty regarding the contribution of host, agent, environmental, or pharmacological factors. The altered health-seeking behaviour of Indian patients, influenced by the easy availability of drugs, including those containing topical steroids, adds complexity. Dermatophytosis now exhibits increased resilience, higher recurrence rates, and a growing number of patients presenting with chronic or recurrent forms. This situation underscores the necessity for a comprehensive understanding of the evolving landscape of dermatophytosis in India.[1], [2]
Despite dermatologists being vigilant and adapting to the evolving landscape of dermatophytosis, there is a notable lack of emphasis on the quality of life (QoL) of patients. While it is acknowledged that superficial dermatophytosis contributes to social embarrassment and stress, the extent of its impact on patients' QoL has not been thoroughly evaluated or comprehended by dermatologists. 2Recognizing the psychological burden and need to evaluate the QoL in individuals with fungal infections is necessary to understand the extent of its influence.
The relationship between dermatology and psychiatry can be emphasised as one can significantly influence the other .Minor alterations in the surface of the skin can cause minimal distress, stress and can cause to an extent of anxiety disorders or depression to an individual on ones perception of the condition. It can ultimately influence the quality of life of an individual. [3], [4], [5]
Aims and Objectives
Primary
To evaluate depression in patients with dermatophyte infections at a tertiary care hospital.
Secondary
To assess the severity of depression and its association with dermatophyte infections.
Materials and Methods
This is a cross sectional observational study which will be conducted over a period of (6) months from June 2023 to November 2023 inclusive of all patients with dermatophyte infections who have come for first consultation to the department of dermatology at Adichunchanagiri hospital and research centre, or have come for follow-up visits. The subjects will be informed about the nature and procedure of the study, following which written consent will be obtained. After the collection of basic demographic details like age, sex, and occupation, a detailed history will be taken which includes age at the onset of fungal infection, age at the time of initial treatment of fungal infection, family history of fungal infection using semi structured questionnaire. A thorough dermatological examination of the face and body will be done to look for the extent of lesions.
In this study the patients were recruited through convenience sampling and the inclusion criteria was patients diagnosed as having cutaneous fungal infection by the consultant dermatologist after clinical evaluation. All the patients were informed about the nature of study and its applications and verbal informed consent was obtained from patients who were willing to participate in the study.
All patients will be asked to fill up DLQI questionnaire, [6] first introduced by Finlay and Khan, in 1994 which is used as a study instrument for this study.
The DLQI is a validated questionnaire that grades quality of life by evaluating the following domains: (a) physical symptoms and feelings (questions 1 and 2), (b) daily activities (questions 3 and 4), (c) leisure (questions 5 and 6), (d) work/school (questions 7), (e) personal relationships (questions 8 and 9), and (f) treatment (question 10). Each question is scored as "very much" (score 3), "a lot" (score 2), "a little" (score 1), and "not at all" (score 0), keeping in mind the problems faced the previous week due to the disease.
Final DLQI score is the sum of all scores (range 0-30). High scores indicate poor QoL.
DLQI score is interpreted as follows:
No effect on patient's life
2-5 small effect on patient's life
6-10 moderate effect on patient's life
11-20 very large effect on patient's life
21-30 extremely large effect on patient's life. [1]
Screening for the prevalence and assessment of severity of depression in patients with fungal infections will be done by application of Hospital Anxiety and Depression scale (HADS) [7] and Beck’s Depression Inventory (BDI). [8]
Those who are found to have severe psychiatric morbidity or suicidal ideation during the course of the study shall be referred to the department of Psychiatry for further management.
Based on the questionnaire rating scale answered, the scores were totaled and results tabulated. The data were entered and analyzed using SPSS 20.0 software for frequency distribution, descriptive analysis, spearman’s rho and chi square test to assess depression, anxiety and quality of life and their correlation among the subjects.
Study size
All patients presenting with fungal infections in the department of Dermatology in Adichunchanagiri hospital and research centre, BG Nagara during the study period. In cases where the patient is less than 18 years of age consent was taken from the primary caregiver.
Inclusion criteria
All patients aged above 16 years with fungal infections who visit the dermatology OPD at AHRC, BG Nagara and who are willing to participate in the study.
Exclusion criteria
Patients with fungal infections who are not willing to participate in the study.
Patients aged below 16 years.
Patients with any other dermatological comorbidity.
Pregnant and lactating women
Patients with secondary bacterial infection
Patients on antifungal therapy (oral, topical, systemic) in the last 4 weeks.
Patients in immunocompromised states or who were on intake of systemic immunosuppressant within the past 14 days.
Patients with a history of known psychiatric illness.
Patients with chronic medical illnesses such as heart, pulmonary and joint diseases, diabetes and epilepsy that affect their mental status.
Patients who used topical or systemic medicines like anabolic steroids, corticosteroids, corticotrophin, phenytoin, phenobarbital, lithium, isoniazid, iodides, bromides, cyclosporine and azathioprine within 1 month.
Ethical consideration
Written informed consent has been documented for all subjects before their participation in the study.
This study does not include any active interventions that might be of possible risk to the subjects.
Subjects who are found to be severely depressed or those with active suicidal ideation will be admitted under the department of psychiatry and treated accordingly.
Results
A total of 183 cutaneous manifestations of dermatophytosis were observed. Among the patients surveyed, 88 were male (48.1%), and the remaining 95 (51.9%) were female. Among these patients, 135 were married (73.77%), and 48 were unmarried (26.22%). The highest incidence was seen in the third to sixth decades of life, with the age of onset being more than 35 years of age in 112 patients (61.2%). Only 11 patients were ill-literate (6.01%), 12 attended primary school (6.5%), 110 completed the 10th standard (60.1%), and 50 were graduates (27.32%).
Among the patients considered in this study, 31 (16.93%) had comorbid conditions such as diabetes, hypertension, and hypothyroidism. 17 individuals had a history of substance use, predominantly alcohol, and 3 had a history of both smoking and consuming alcohol. Reportedly, the duration of illness was between one and six months for the majority, amounting to 84 patients (45.9%); 56 patients (30.6%) had been suffering for more than six months, and the remaining for less than one month.
All of the patients presented with the chief complaint of itchy lesions varying in their distribution, with 44 patients (24%) presenting with lesions above waist, 84 below waist (45.9%), and 53 patients having extensive lesions covering the entire length of their bodies (28.96%); 66 patients had these lesions in the groin area (36%). A history of poor hygiene was noted; 41 had a history of contact with domestic animals mainly through cattle rearing (22.4%), 25 of them had contact with mud through farming practices (13.66%), and 85 patients did not bathe daily (46.44%).
|
Parameters |
Frequency |
Percentage |
|
Gender |
|
|
|
Male |
88 |
48.1 |
|
Female |
95 |
51.9 |
|
Age |
|
|
|
Less than 21 years |
22 |
12.0 |
|
21 to 35 years |
46 |
25.1 |
|
More than 35 years |
115 |
62.8 |
|
Age of onset |
|
|
|
Less than 21 years |
29 |
15.8 |
|
21 to 35 years |
42 |
22.9 |
|
More than 35 years |
112 |
61.2 |
|
Education |
|
|
|
Ill-literate |
11 |
6.0 |
|
Primary school |
12 |
6.5 |
|
Matriculate |
110 |
60.1 |
|
Graduate |
50 |
27.3 |
|
History of comorbidity |
|
|
|
Present |
31 |
16.9 |
|
Absent |
152 |
83.0 |
|
History of substance abuse |
|
|
|
Present |
17 |
9.2 |
|
Absent |
166 |
90.7 |
|
Duration of illness |
|
|
|
Less than 1 month |
43 |
23.4 |
|
1 month to 6 months |
84 |
45.9 |
|
More than 6 months |
56 |
30.6 |
|
Distribution of lesions |
|
|
|
Above waist |
46 |
25.1 |
|
Below waist |
84 |
45.9 |
|
Both |
53 |
28.9 |
|
History of contact with mud |
|
|
|
Present |
25 |
13.6 |
|
Absent |
158 |
86.3 |
|
History of contact with animals |
|
|
|
Present |
41 |
22.4 |
|
Absent |
142 |
77.5 |
|
Frequency of bathing |
|
|
|
Daily |
98 |
53.5 |
|
Irregular |
85 |
46.4 |
|
HADS (Anxiety) |
|
|
|
Normal |
151 |
82.5 |
|
borderline abnormal |
27 |
14.7 |
|
Abnormal |
5 |
2.7 |
|
HADS (Depression) |
|
|
|
Normal |
162 |
88.5 |
|
Borderline abnormal |
19 |
10.3 |
|
Abnormal |
2 |
1.0 |
|
DLQI |
|
|
|
No effect on patient’s life |
8 |
4.3 |
|
Minimal effect |
83 |
45.3 |
|
Moderate affect |
71 |
38.7 |
|
Very large affect |
21 |
11.4 |
|
BDI |
|
|
|
Minimal depression |
153 |
83.6 |
|
Mild depression |
16 |
8.7 |
|
Moderate depression |
7 |
3.8 |
|
Severe depression |
7 |
3.8 |
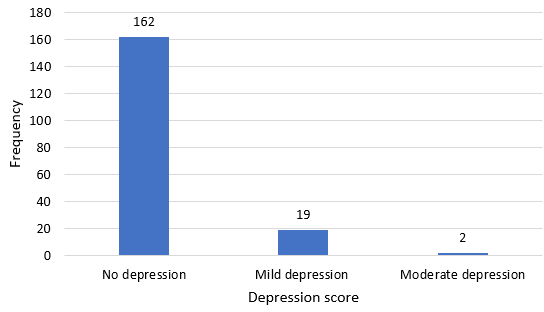
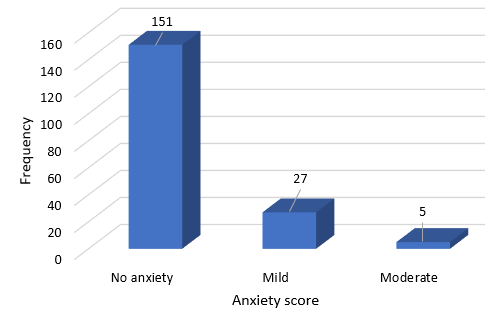
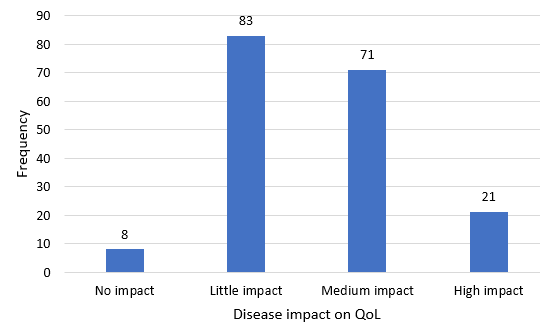
The Hospital Anxiety and Depression Scale (HADS) was applied to screen for anxiety and depression, and 27 of them were found to have borderline abnormal anxiety (14.8%), while 5 were found to have abnormal levels of anxiety (2.7%); likewise, 19 patients were found to have borderline abnormal (10.4%) levels of depression, while 2 of them had abnormal levels of depression (1.1%). The severity of depression was assessed using Beck’s Depression Inventory, and it was found that a majority, corresponding to 153 patients, had minimal depression (83.6%), 16 patients had mild depression (8.7%), and the occurrence of moderate and severe depression was identical at 3.8% each. The dermatological quality of life index was employed to evaluate the impact on quality of life, and it was found that a majority of the patients’ QoL was minimally affected (45.4%), 71 of them were moderately affected (38.8%), and only 21 were very largely affected (11.5%). ([Table 1])
Incidence of dermatophytosis, and anxiety and depression were found to show monotonic positive correlation, sequentially the impact of their severity on the quality of life was found to be statistically significant. ([Figure 1], [Figure 2], [Figure 3])
Discussion
Psychodermatology is an interdisciplinary field that explores the intricate relationship between the mind and the skin. It acknowledges the bidirectional influence between the mind and the skin, recognizing that emotional and psychological states can impact the onset, severity, and course of skin disorders, while skin conditions, in turn, can affect an individual's psychological well-being and quality of life. Dermatophytosis is the most widespread fungal infection of skin, nail, hairs, and affect 40 million human population worldwide, in various forms. In the recent few years in India, the prevalence of dermatophytosis has been consistently rising, ranging from 36% to 78%. [3], [4] Depression in the context of fungal infections represents a complex and multifaceted interaction between mental health and physical illness. Fungal infections, which can affect various parts of the body, have been associated with an increased risk of psychological distress, including depression, due to the profound impact these conditions can have on an individual's overall well-being. Depression in patients with fungal infections represents a significant and often overlooked aspect of their overall well-being. The psychological toll of these conditions, including the potential onset or exacerbation of depression, is equally noteworthy.
Approximately 30-40% patients seeking treatment for skin disorders have an underlying psychiatric or a psychological problem that either causes or exacerbates a skin complaint [5] and evidence suggests that the course of many skin disorders is affected by stress and psychological events. [9]
In our study, the gender distribution was nearly equal but a large number of patients were found to be from the rural background owing to the study location, could in turn be linked to poor socioeconomic status, surmounting to financial burden on the family, and hindering the long-term treatment required for their illnesses. Lack of literacy and graduate level education can further precipitate the recurrence rates in terms of awareness, understanding of the illness and need for appropriate compliance with treatment. Significant majority of the patients were married which could be the positive influence on mental health status of the patients, as only a minority were found to have both abnormal levels of anxiety and depression. However, these percentages were found to be higher in females, which could be due to lack of social support and existing gender norms pertaining to physical appearances. They also report feeling of helplessness, embarrassment, and self-consciousness. They can have vicious cycle of despair due to the adverse emotional effect resulting from severe disease and physical discomfort or pain, which are often undermined by others. These findings were consistent with the results of previous studies. [10], [11], [12]
There were a significant number of hypothyroidism cases, 6 out of 31 who were found to be suffering from medical comorbidities (19.35%). Additionally the extent of the lesions and their distribution pattern, history of poor hygiene and substance use had not been considered in the previous studies. In acknowledging the influence of these elements, the impact on quality of life could be ascertained. However, the correlation with dermatophytosis and anxiety and depression was weak which can possibly explained by the duration of illness which was less than 6 months in majority of our subjects and all of the participants were recruited from those consulting in the outpatient department of dermatology. Furthermore, previous studies results reflect only the presence of anxiety and depression and not the severity of depression.[13], [14], [15]
Our study has focused on only dermatophytosis while several other dermatological diagnoses are rampant and have glaring consequences on the mental health and well-being. The study population is limited to those who voluntarily reported to the hospital outpatient department. While anxiety and depression compound as utmost psychiatric issues, the incidence and association of other psychiatric conditions with dermatological ailments remains to be explored. Long term follow-up of these patients would help in appreciating the dynamics and variations of the said presentations and thereby planning and implementing psychotherapeutic interventions in favour of psychodermatology.
Conclusion
This study addresses the impact of quality of life and mental health of individuals who are affected by fungal infections in a rural population. By assessing depression severity using validated instruments, the research unveiled the multidimensional nature of the dermatophyte infections.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s legal guardian has given the consent for images and other clinical information to be reported in the journal. The patient’s legal guardian understands that name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Source of Finding
None.
Conflicts of Interest
There are no conflicts of interest
References
- Panda S, Verma S. The menace of dermatophytosis in India: The evidence that we need. Indian J Dermatol Venereol Leprol. 2017;83(3):281-4. [Google Scholar]
- Laxmi H, Dilip N, Shashikiran A. The impact of superficial dermatophytosis on quality of life: A cross-sectional observational study. IP Indian J. 2021;7(3):191-6. [Google Scholar]
- Misery L, Schut C, Balieva F, Bobko S, Reich A, Sampogna F. White paper on psychodermatology in Europe: A position paper from the EADV Psychodermatology Task Force and the European Society for Dermatology and Psychiatry (ESDaP). J Eur Acad Dermatol Venereol. 2023;37(12):2419-27. [Google Scholar]
- Christensen R, Jafferany M. Psychiatric and psychologic aspects of chronic skin diseases. Clin Dermatol. 2023;41(1):75-81. [Google Scholar]
- KD, Rathore K, Karde A. Psycho-cutaneous disorders: a comprehensive analysis in psychiatric and dermatology patients. J Popl Ther Clin Pharmacol. 2016;30(18):582-92. [Google Scholar]
- Beck AT, Steer RA, Brown GK. . Beck Depression Inventory (BDI-II). 1996. [Google Scholar]
- Lovibond S, Lovibond P. . Manual for the Depression Anxiety Stress Scales . 1995. [Google Scholar]
- Finlay A, Khan G. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1992;19(3):210-6. [Google Scholar]
- Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: an appraisal. Indian J Dermatol. 2017;62(3):227-36. [Google Scholar]
- Reemabana, Singh M, Sumeet D, Saini P, Sharma K, D. Original Research Prevalence of anxiety and depression in patients with tinea in a tertiary care centre. Int J Life Sci Biotechnol Pharm Res. 2024;13(2):344-7. [Google Scholar]
- Tripathi A, Meher S, Sharma SK, Gupta R, Sami U, Mahajan R. Skin Diseases in Patients With Primary Psychiatric Conditions in Northern India: A Cross-Sectional Study. Curēus. 2024;16(2). [Google Scholar] [Crossref]
- Girisha B, George A, Rao S. A perspective study of cutaneous manifestations in primary psychiatric disorders in a tertiary care hospital. Indian J Psychiatry. 2018;60(2):213-6. [Google Scholar]
- Naglot A, Shrimali D, Nath B, Gogoi H, Veer V. Recent Trends of Dermatophytosis in Northeast India (Assam) and Interpretation with Published Studies. Int J Curr Microbiol App Sci. 2015;4(11):111-20. [Google Scholar]
- Picardi A, Abeni D, Melchi C, Puddu P, Pasquini P. Psychiatric morbidity in dermatological outpatients: An issue to be recognized. Br J Dermatol. 2000;143(5):983-91. [Google Scholar]
- Humphreys F, Humphreys M. Psychiatric morbidity and skin disease: what dermatologists think they see. Br J Dermatol. 1998;139(4):679-81. [Google Scholar]
How to Cite This Article
Vancouver
Johnson RA, HK TP, Swaroop MR, R M, KS K, K SPH. Depression and quality of life among patients with dermatophyte infections at a rural tertiary care hospital-A cross sectional study [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Oct 21];11(1):33-38. Available from: https://doi.org/10.18231/j.ijced.2025.005
APA
Johnson, R. A., HK, T. P., Swaroop, M. R., R, M., KS, K., K, S. . P. H. (2025). Depression and quality of life among patients with dermatophyte infections at a rural tertiary care hospital-A cross sectional study. IP Indian J Clin Exp Dermatol, 11(1), 33-38. https://doi.org/10.18231/j.ijced.2025.005
MLA
Johnson, Richin Anna, HK, Tejaswi Prithviraj, Swaroop, M R, R, Monisha, KS, Karthick, K, Surakshitha Poornima H. "Depression and quality of life among patients with dermatophyte infections at a rural tertiary care hospital-A cross sectional study." IP Indian J Clin Exp Dermatol, vol. 11, no. 1, 2025, pp. 33-38. https://doi.org/10.18231/j.ijced.2025.005
Chicago
Johnson, R. A., HK, T. P., Swaroop, M. R., R, M., KS, K., K, S. . P. H.. "Depression and quality of life among patients with dermatophyte infections at a rural tertiary care hospital-A cross sectional study." IP Indian J Clin Exp Dermatol 11, no. 1 (2025): 33-38. https://doi.org/10.18231/j.ijced.2025.005
