- Visibility 392 Views
- Downloads 68 Downloads
- Permissions
- DOI 10.18231/j.ijced.2025.019
-
CrossMark
- Citation
Exploring the spectrum: A case report of acquired bilateral nevus of Ota-like macules (ABNOM) with mucosal involvement
Abstract
Acquired Bilateral Nevus of Ota like Macules (ABNOM) typically presents in adulthood with bilaterally symmetrical blue-brown to slate-gray macules in a speckled distribution over the face. Mucosal pigmentation is characteristically absent. Dermoscopy is a non-invasive tool that aids in distinguishing ABNOM from Melasma. Laser therapy is the most widely used treatment modality. Here we present the case of an 18-year-old female diagnosed as ABNOM with Mucosal involvement.
Introduction
Acquired Bilateral Nevus of Ota-like Macules, also known as Hori’s Nevus, is a type of dermal melanocytosis primarily seen in females after the third decade of life. [1] Lack of mucosal involvement has been thought to be a crucial distinction for Hori's nevus. Though they are seldom reported, a few cases of Hori's nevus with accompanying ocular pigmentation have been investigated. [2] Owing to the paucity of research on this perspective, we are reporting here a case of an 18-year-old North Indian female patient diagnosed as ABNOM with Mucosal involvement.
Case Report
An 18-year-old North Indian female presented to our dermatology out-patient department with a complaint of bluish discoloration over the left cheek since birth. It initially started as a pea sized lesion below the left eye and gradually increased in size over the years to the current size extending over the entire left cheek. The lesion also became darker in color. She also had two similar linear and pin head sized blue colored lesions over the white area of the left eye that are present since birth. There is no involvement of the right eye. Since the past five to six years, the patient noted that similar round, pea sized, bluish-gray lesions were also appearing on the right cheek. These lesions are also progressively increasing in size. The lesions are completely asymptomatic. The patient does not have any visual complaints like blurring of vision or any associated symptoms. No family history of similar lesions is known.
|
Features |
Abnom |
Bilateral nevus of OTA |
Melasma |
Riehl’s melanosis |
Our case |
|
Onset |
Middle aged, few reports in adolescence |
At birth or during the first year of life |
20-40 years of age |
Middle age |
Noticed at birth with progression during adolescence |
|
Gender Predilection |
Females |
Females |
Females (90% cases) |
Females |
Female |
|
Clinical presentation |
Multiple blue-brown or slate gray macules present in a speckled pattern, distributed symmetrically over the bilateral malar region, forehead, temples, eyelids and/or nose |
Patchy and superficial brown pigmentation following a reticular or geographical pattern; diffuse and deeper blue pigmentationin a speckled pattern |
Symmetrical, reticulated, hyperpigmented macules and patches with irregular borders present on the centrofacial, malar and mandibular region |
Brown-gray pigmentation favoring site of application of contactants, especially cosmetics |
Multiple well demarcated bluish-gray macules in a speckled distribution over the bilateral malar areas of the face |
|
Mucosal involvement |
Usually absent |
Present |
Absent |
Absent |
Present |
|
Dermoscopy |
Speckled homogeneous pattern with a blue-brown or gray color |
Brown and gray structureless areas with a patchy distribution and scattered brown- gray dots |
Arc-shaped or circular, regular or irregular, light brown network that spares the sweat gland openings or follicles[3] |
Pseudonetwork patterns with brown/gray dots/globules grouped in an arcuate, semiarcuate, or hexagonal way |
Speckled homogeneous pattern with blue gray discoloration |
|
Histology |
Irregularly shaped, bipolar melanocytes dispersed in the papillary and mid dermis, particularly in the subpapillary dermis, without disrupting normal skin architecture |
Elongated dendritic melanocytes scattered in the superficial dermis, occasionally extending deeper; Melanophages are seldom present |
Melanocytes are enlarged and more dendritic, number is not increased; reflected by increased melanin deposition in the epidermis and dermis[4] |
Vacuolar degeneration of basal layer of epidermis and a perivascular or band‐like dermal infiltrate with pigmentary incontinence; many melanophages in the upper dermis |
Refused by the patient |
|
Year |
Reference |
Title |
Results |
|
2022 |
Rattananukrom T. et al. [3] |
A Comparative Study of Dermatoscopic Features of Melasma and Hori's Nevus in Asian Patients |
- 46 patients; - Common features of Hori’s nevus: Blue-brown/grey pigmentation and speckled homogenous pattern |
|
2017 |
Zhang, Q. et al. [2] |
Clinical profile and triggering factors for acquired, bilateral nevus of Ota-like macules |
- 102 cases; - Speckled macules on the face; Coexisted with patchy lesions or a band-like pigmentation - 52.0% cases had sclera pigmentation |
|
2014 |
Bhat RM. et al. [5] |
Acquired Bilateral Nevus of ota-like Macules with Mucosal Involvement: A New Variant of Hori's Nevus |
- Case report; 42-year-old male - Bilaterally symmetrical blue-brown to slate-gray speckled macules over the face - Conjunctival, scleral, and hard palate mucosal pigmentation present |
|
1987 |
Sun CC. et al. [1] |
Naevus fusco-caeruleus zygomaticus |
- 110 cases - Unusual type of naevus: Naevus fusco-caeruleus zygomaticus were studied |
|
1984 |
Hori Y. et al. [6] |
Acquired, bilateral nevus of Ota-like macules |
-First study to describe the clinical features and histopathology of ABNOM in 22 Japanese patients (M:F = 1:21) |


Upon clinical examination, multiple well demarcated bluish-gray macules ranging from 0.2-1 cm in diameter were present in a speckled distribution with an asymmetrical pattern over the bilateral malar areas of the face ([Figure 1]). On the left malar area, the macules have coalesced to form a bluish gray patch of size 3x4 cm ([Figure 2]).
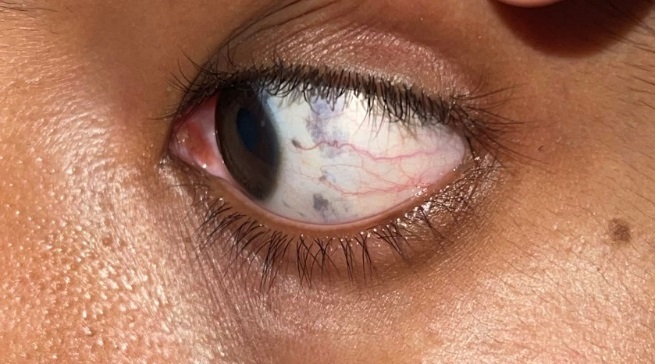
On ocular examination, the left sclera exhibits multiple dark blue colored macules ([Figure 3]). These are arranged linearly extending from 12’o clock to 6’o clock position over the left side, 0.7 cm away from the pupil. A single blue macule of 0.3cm diameter is also present on the sclera at the 10’o clock position of the left eye. An ophthalmoscopic examination revealed no further abnormalities. Otoscopic and oral cavity examination did not reveal any significant findings.
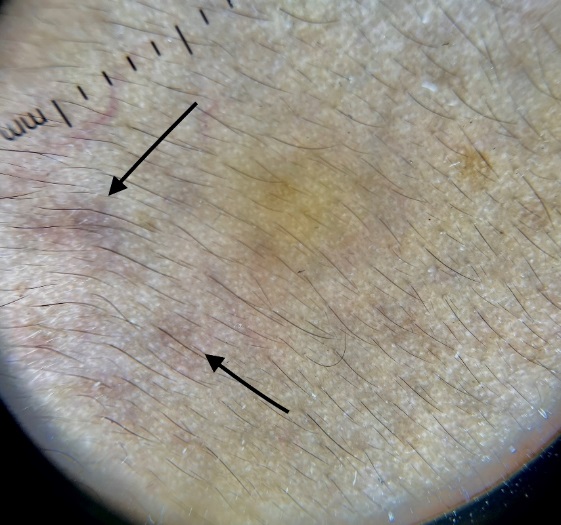
On dermoscopy, speckled homogenous pattern with blue gray discoloration is seen over the areas of pigmentation on the bilateral malar areas ([Figure 4]). Histopathological examination was advised but was refused by the patient.
Based on the clinico-dermoscopic evaluation, a diagnosis of Acquired Bilateral Nevus of Ota like Macules (ABNOM) with Mucosal Involvement was made. The patient was advised 1064nm Q-switched NdYAG Laser for further management which she refused due to monetary concern.
Discussion
Acquired Bilateral Nevus of Ota like Macules (ABNOM) was first described by Hori et al in 1984 as an entity of circumscribed dermal melanocytosis.[6]
Clinically, it manifests as multiple blue-brown and/or slate gray macules present in a speckled pattern, distributed symmetrically over the bilateral malar region, forehead, temples, eyelids and/or nose. It has also been referred to as Nevus fusco-caeruleus zygomaticus based on its clinical appearance. Even though it typically affects middle-aged females of Asian descent, ABNOM has been reported to manifest in adolescence, as was the case in our instance.[1], [2]
The name "ABNOM" comes from its histological resemblance to Nevus of Ota.
As the diagnosis is usually clinical, Nevus of Ota can be distinguished from Hori's nevus due to its later onset, speckled distribution pattern, and bilateral involvement. Lack of mucosal involvement, unlike Nevus of Ota, is a defining attribute of Hori's nevus.[7], [5]
The key differentials for ABNOM include bilateral nevus of Ota, melasma and Riehl’s melanosis which have been summarized in [Table 1].
The most prevalent modalities for treating Hori's nevus are laser therapy, which works on the principle of selective photothermolysis, and dermabrasion, which is less common. Of the several types of lasers, the most commonly used ones are QS:NYL, QSAL, ER:YAG, QSRL, and CO2 laser. [8]
While the absence of mucosal involvement is thought to be a key characteristic that sets ABNOM apart from bilateral nevus of ota, a study done in 2017 observed that 52% of individuals had associated scleral pigmentation with ABNOM, a finding similar to our case which is often disregarded. [6]
Taking into account the bilateral involvement, onset prior to adolescence, speckled blue gray pattern, and scleral pigmentation, a diagnosis of ABNOM with mucosal involvement was made ([Table 2]).
Conclusion
Our case study, by demonstrating onset in adolescence and the presence of scleral pigmentation, illustrates the diversity in the presentations of ABNOM, highlighting the significance of identifying its distinctive characteristics for appropriate management.
Statement of Responsibility
We, Dr. Aneesha Puri, Dr. Shitij Goel, Dr. Kritika Bansal and Dr. Isha Singla, collectively affirm our substantial contributions to the conception, design, acquisition, analysis, and interpretation of the data presented in this case report. Additionally, each author has been actively involved in drafting the manuscript and critically revising it for intellectual content. We stand by the accuracy and integrity of the work and take responsibility for all aspects of its creation and dissemination.
Conflict of Interest
None.
Source of Funding
None.
References
- Sun C, Lü Y, Lee E, Nakagawa H. Naevus fusco-caeruleus zygomaticus. Br J Dermatol. 1987;117(5):545-53. [Google Scholar]
- Zhang Q, Jiang P, Tan C, Yang G. Clinical profile and triggering factors for acquired, bilateral nevus of Ota-like macules. Cutan Ocul Toxicol. 2017;36(4):327-30. [Google Scholar]
- Baykal C, Yılmaz Z, Sun GP, Büyükbabani N. The spectrum of benign dermal dendritic melanocytic proliferations. J Eur Acad Dermatol Venereol. 2019;33(6):1029-41. [Google Scholar]
- Rattananukrom T, Suchonwanit P, Thadanipon K, Vachiramon V. A Comparative Study of Dermatoscopic Features of Melasma and Hori's Nevus in Asian Patients. J Clin Aesthet Dermatol. 2022;15(3):16-20. [Google Scholar]
- Bhat R, Pinto H, Dandekeri S, Ambil S. Acquired Bilateral Nevus of ota-like Macules with Mucosal Involvement: A New Variant of Hori's Nevus. Indian J Dermatol. 2014;59(3):293-6. [Google Scholar]
- Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984;10(6):961-4. [Google Scholar]
- Wang R, Ko D, Friedman B, Lim H, Mohammad T. Disorders of hyperpigmentation. Part I. Pathogenesis and clinical features of common pigmentary disorders. J Am Acad Dermatol. 2023;88(2):271-88. [Google Scholar]
- Kaur H, Sarma P, Kaur S, Kaur H, Prajapat M, Mahendiratta S. Therapeutic options for management of Hori's nevus: A systematic review. Dermatol Ther. 2020;33(1). [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Puri A, Goel S, Bansal K, Singla I. Exploring the spectrum: A case report of acquired bilateral nevus of Ota-like macules (ABNOM) with mucosal involvement [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Oct 05];11(1):126-129. Available from: https://doi.org/10.18231/j.ijced.2025.019
APA
Puri, A., Goel, S., Bansal, K., Singla, I. (2025). Exploring the spectrum: A case report of acquired bilateral nevus of Ota-like macules (ABNOM) with mucosal involvement. IP Indian J Clin Exp Dermatol, 11(1), 126-129. https://doi.org/10.18231/j.ijced.2025.019
MLA
Puri, Aneesha, Goel, Shitij, Bansal, Kritika, Singla, Isha. "Exploring the spectrum: A case report of acquired bilateral nevus of Ota-like macules (ABNOM) with mucosal involvement." IP Indian J Clin Exp Dermatol, vol. 11, no. 1, 2025, pp. 126-129. https://doi.org/10.18231/j.ijced.2025.019
Chicago
Puri, A., Goel, S., Bansal, K., Singla, I.. "Exploring the spectrum: A case report of acquired bilateral nevus of Ota-like macules (ABNOM) with mucosal involvement." IP Indian J Clin Exp Dermatol 11, no. 1 (2025): 126-129. https://doi.org/10.18231/j.ijced.2025.019
