- Received December 08, 2024
- Accepted January 14, 2025
- Publication February 08, 2025
- Visibility 6 Views
- Downloads 1 Downloads
- DOI 10.18231/j.ijced.2025.020
-
CrossMark
- Citation
Facial port wine stain with predominant ipsilateral and islands of contralateral oral mucosal involvement: A rare case report
- Author Details:
-
Samuel Jeyaraj Daniel
-
Balaji Ganesh Jayaraman
-
Saranya Selvam
-
Rosemin Jose Meleth *
Introduction
Portwine stains are congenital capillary malformations with varying topographic patterns and vivid margins. Recent studies have shown that it results from differentiation-impaired endothelial cells in human skin with a progressive dilatation of immature venule-like vasculatures.[1] A prospective study has proposed an incidence of 0.7% for PWS in new born. [2] PWS initially appears as flat red macules in childhood, as age advances, they become more hyperpigmented with soft tissue hypertrophy and by middle age, often become raised as a result of the development of vascular nodules that are susceptible to spontaneous bleeding or haemorrhage.[3], [4] Patients with facial PWS often demonstrates a spectrum of oral manifestation. The most common oral manifestations previously reported were enlargement of the lip (53.3%), stained gums (46.7%), abnormal bite (30%) and spontaneous bleeding of the gums (26.7%).[5] This case report highlights a unique morphological variation of mucosal staining in a patient with facial portwine stain.
Case Report
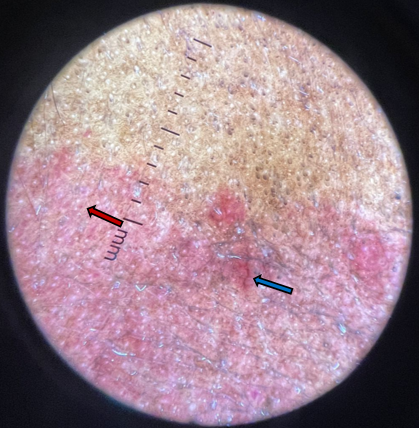
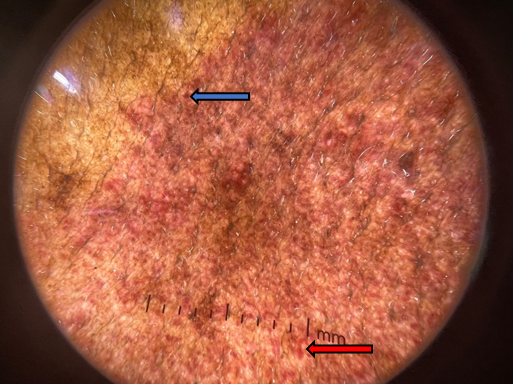
A 60year old male presented with reddish discoloration of skin over right side of the face which has been present since birth and has progressively increased in size over the years. There was no past history of seizures, hemiparesis or vision abnormalities. On dermatological examination there was well demarcated erythematous plaque over right side of face involving the upper lip, maxillary, mandibular, periorbital and temporal region which spanned over all the three divisions (V1,V2 & V3) of trigeminal nerve [[Figure 1]]. Multiple hyperpigmented discrete and coalescing nodules were noted over maxillary and zygomatic region [[Figure 1], [Figure 2]]. There was right sided hemihypertrophy of face [[Figure 1]]. Examination of oral mucosa revealed bright red patches over right side of tongue with few areas of sparing over the lateral aspect and red macular islands on left side of tongue [[Figure 3], [Figure 4]]. Right palatal and buccal mucosa had similar red patches not crossing the midline [[Figure 4]]. Soft tissue hypertrophy of right side of palate was also noted [[Figure 3]]. General examination did not reveal any abnormality of limb length, girth and dilated tortuous veins. System examination was normal. Dermoscopy of the lesion revealed dot vessels, globules vessels, linear vessels and sausage vessels [[Figure 5], [Figure 6]]. Patient was referred for a neurological and ophthalmological evaluation but was eventually lost to follow up.
|
S.No |
Author |
Skin involvement with Dermatome |
Oral mucosal involvement |
Year |
|
1 |
Namrata C gill et al |
Left Facial PWS V1& V2 |
Ipsilateral staining of palate |
2010 |
|
2 |
Tripathi K et al |
Right Facial PWS V1 & V2 |
Ipsilateral hyperplastic lesions on right side of maxilla |
2015 |
|
3 |
Shahid M sheikh et al |
Right Facial PWS V1,V2 & V3 C1 to C3 |
Ipsilateral staining of palate |
2015 |
|
4 |
Medhini Madie et al |
Right Facial PWS V1& V2 |
Ipsilateral staining of buccal mucosa and soft palate with pyogenic granuloma |
2017 |
|
5 |
Medhini Madi et al |
B/L Facial PWS V1, V2& V3 C1 to C6 |
B/L staining of soft palate, labial and buccal mucosa |
2017 |
|
6 |
Narender Reddy B et al |
B/L Facial PWS , V3 |
B/L mucosal staining on the floor of the mouth, ventral surface and tip of the tongue and right side of the palate |
2018 |
|
7 |
Sasti Priya et al |
Right Facial PWS V3 |
Ipsilateral mucosal staining on ventral aspect of tongue with pyogenic granuloma |
2023 |
|
8 |
Present case report |
Right Facial PWS , V1,V2 & V3 |
Predominant ipsilateral staining of palate, buccal mucosa, and tongue, with unique red macular islands of lingual mucosa on the contralateral side |
2024 |




Discussion
Facial portwine stains are unique birthmarks most commonly involving maxillary and mandibular division of trigeminal nerve. Majority of PWS lesions are unilateral and follow the typical distribution of the trigeminal nerve. A study of 310 PWS patients, 32% had lesions in the area supplied by the maxillary (V2) branch of the trigeminal nerve, 41% had lesions involving both the ophthalmic (V1) and maxillary (V2) branches, 5% had lesions in the combined maxillary (V2) and mandibular (V3) branches, and 10% had lesions across all three branches [13] PWS can be an isolated manifestation or can be associated with other congenital vascular malformations such as SWS (Sturge weber syndrome), Parkes-Weber syndrome, Klippel -Trenauny syndrome, Proteus syndrome and arteriovenous malformation. When associated with SWS they can present with various neural and ocular manifestations namely leptomenigeal angiomatosis and glaucoma.[14] As age advances many secondary changes are noted over these lesions namely fibrovascular nodules, cutaneous thickening, soft tissue hypertrophy and pyogenic granuloma. Dermoscopy of the PWS in this case showed varying morphology of blood vessels namely dot vessels, globule vessels, linear vessels and sausage vessels. It is helpful to differentiate PWS from other vascular diseases such as telangiectasia, angioma serpiginosum and angiokeratoma. [15] The orodental manifestations were more frequently observed among patients with darker and thicker PWS. [5]
Oral manifestation reported so far in literature are commonly ipsilateral involvement of oral mucosa. Ipsilateral involvement of oral mucosa when traced embryologically is attributed to segmental development of vascular channels during embryogenesis.[16] The red macular islands on opposite side in this case can be due to aberrant vasculogenesis during embryonic development. Predominant ipsilateral mucosal staining of the palate, buccal mucosa, and tongue, interspersed with unique contralateral lingual mucosal red macular islands as noted in our case is seldom documented in literature.
Conclusion
The prominent skin manifestation is a key characteristic in patients with port-wine stains (PWS), leading to initial consultations with dermatologists. It is essential for the treating clinician to be aware of this distinct pattern of mucosal staining in PWS to ensure timely identification and to seek appropriate interdisciplinary advice for further management.
Source of Funding
None.
Conflict of Interest
None.
References
- W Tan, J Wang, F Zhou, L Gao, Y Rong, H Liu. Coexistence of Eph receptor B1 and ephrin B2 in port-wine stain endothelial progenitor cells contributes to clinicopathological vasculature dilatation. Br J Dermatol 2017. [Google Scholar]
- L Techasatian, V Sanaphay, P Paopongsawan, LA Schachner. Neonatal Birthmarks: A Prospective Survey in 1000 Neonates. Global Pediatric Health 2019. [Google Scholar] [Crossref]
- RG Geronemus, R Ashino. The medical necessity of evaluation and treatment of port-wine stains. J Dermatol Surg Oncol 1991. [Google Scholar]
- WF Lever, G Schaumburg-Lever. . Histopathology of the Skin 1990. [Google Scholar]
- MB Dowling, Y Zhao, DH Darrow. Orodental manifestations of facial port-wine stains. J Am Acad Dermatol 2012. [Google Scholar]
- NC Gill, N Bhaskar. Sturge – Weber syndrome: A case report. Contemp Clin Dent 2010. [Google Scholar]
- AK Tripathi, V Kumar, R Dwivedi, C S Saimbi. Sturge-Weber syndrome: oral and extra-oral manifestations. BMJ Case Rep 2015. [Google Scholar] [Crossref]
- M Madi, SG Babu, S Achalli, R Castelino. Oral pyogenic granuloma in a port-wine stain A rare co-occurrence. SRM J Res Dent Sci 2017. [Google Scholar]
- M Madi, SuG Babu, S Achalli, S Bhat. A rare bilateral presentation of port wine stain of the face and neck. Cukurova Med J 2017. [Google Scholar]
- BN Reddy, SA Ahmed, DR Shravan Kumar, M Vanje, V Pantala. Congenital Port-Wine Stains affecting Face and Neck region: A rare entity with review of literature . J Oral Med Oral Surg Oral Pathol Oral Radiol 2018. [Google Scholar]
- SM Shaikh. Sturge-Weber Syndrome: A Case Report. JNMA J Nepal Med Assoc 2015. [Google Scholar]
- S Priya, KR Mohan, RP Thangavelu, SM Fenn, K Appusamy. Concurrent Occurrence of Lobular Capillary Haemangioma and Port-Wine Stain: A Case Report and Literature Review. Cureus 2023. [Google Scholar] [Crossref]
- B Tallman, OT Tan, JG Morelli, J Piepenbrink, TJ Stafford, S Trainor. Location of port-wine stains and the likelihood of ophthalmic and/or central nervous system complications. Pediatrics 1991. [Google Scholar]
- OA Sherwani, PC Patra, SA Ahmad. Sturge-Weber Syndrome: A Report of a Rare Case. Cureus 2023. [Google Scholar] [Crossref]
- Y Huang, J Yang, Z Li, L Zhang, L Sun, M Bi. Dermoscopic features of port-wine stains: A study of 264 cases. Australas J Dermatol 2020. [Google Scholar]
- A Graham, JPJM Hikspoors, RH Anderson, WH Lamers, SD Bamforth. Arevised terminology for the pharyngeal arches and the archarteries. J Anat 2023. [Google Scholar]
